Introduction - How to use this virtual patient
Interactive learning exercise on the anti-arrhythmic drug Adenosine.
Learning Objectives
The scenario in this exercise is built on the cardiology "virtual patient" Sally James from the School's Virtual Hospital.
Any comments or questions? Contact: smd-elearning@qmul.ac.uk
Authors: Drs. Ann Chu & Angelo Pieris
E-learning teaching fellows
Barts and the London Medical School, QMUL
Created: 2011
1 - Presentation

Educaiont: University graduate
Occupation: Events manager
You are a surgical F1 on a night shift. Sally James was admitted 24 hours ago with acute appendicitis and underwent a laparoscopic appendicectomy. The operation was uneventful and on the procedure note, the surgeon is aiming for discharge in 1-2 days.
The ward nurse calls you at 10pm. During routine clinical observations, she has noted the following:
HR 200 bpm
BP 115/70
RR 28
SpO2 97% (air)
You ask the nurse to put her on a cardiac monitor and perform an ECG whilst you make your way up to the ward.
1 - Medical history
On further questioning you elicit the following symptoms:
Palpitations - Sally says she can feel her heart racing.
Shortness of breath - Sally says she is finding it hard to breathe.
Chest pain - This is often considered an adverse sign associated with arrhythmias but Sally denies chest pain.
Fainting or feelings of being about to faint - Tachyarrhythmias may be associated with syncope or pre-syncope. Sally says she feels light-headed but has not fainted.
Pins and needles in her hands - This is likely to be associated with tachypnoea and hyperventilation.
With the aid of the notes and a few more quick questions, you establish the following:
• Past Medical History:
24-hours post appendicectomy
No other medical conditions including asthma
• Medications:
Combined oral contraceptive pill
Paracetamol 1g qds
Ibuprofen 200mg tds
Codeine prn
No known drug allergies
• Family history:
Mother – breast cancer undergoing chemotherapy
• Social history:
‘Social smoker’ – average of 5 cigarettes per week
Alcohol – average of 3-4 large glasses of wine per week
Drugs – denies recreational drug use or over-the-counter medications
Works as events manager, lives with 2 housemates
1 - Examination
Whilst asking relevant questions, you are also assessing Sally using the ABCDE approach:
A – airway: patent, speaking in partial to full sentences
B – breathing: tachypnoeic (respiratory rate 28), SpO2 97%, no central/peripheral cyanosis equal air entry, no wheeze or crepitations, no evidence of pulmonary oedema
C – circulation: warm and well perfused, radial and carotid pulses rapid, approx 200bpm, BP maintained at 110/85, heart sounds normal with no added murmurs, JVP not raised
ECG in progress and one pink cannula in situ
D – disability: GCS 15/15, blood sugar 6.2, no obvious neurological deficit
E – exposure: appendectomy wound clean and dry, afebrile, no signs of sepsis
1 - Investigations
The most crucial investigation in this instance is the ECG.
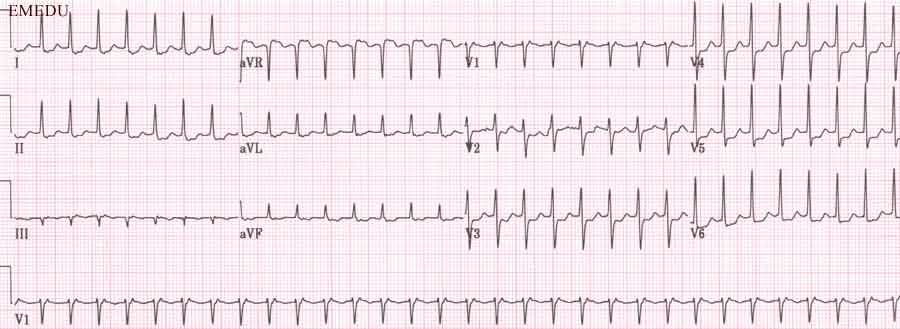
Report the ECG using the following headings:
What practical things should you be doing as a junior doctor in such a situation?
You insert an intravenous line and take blood for various investigations. (E.g. Full Blood Count, Urea &Electrolytes, Clotting screen)
The results will take time to come back and in the meantime you call the medical registrar for help and start management in line with the UK Resuscitation Council Guidelines for a supraventricular tachycardia.
1 - Management

You have already started supporting Sally with initial principles of resuscitation.
Which features would indicate that the patient is unstable? (tick all that apply)
In this case, Sally does not exhibit any adverse features associated with tachyarrhythmias.
What would be your next step in management?
This proves unsuccessful. What could you attempt to use next?
What is the delivery route of the drug ?
IV administration of adenosine is used to transiently block the AV node.
This may terminate a supraventricular arrhythmia or unmask an underlying rhythm.
Give adenosine rapidly via a large vein followed by a rapid saline flush.
Dosing schedules vary – look at your local Trust guidelines. Typical doses can be: 3mg/6mg/9mg or 6mg/6mg/12mg or 6mg/09mg/12mg. These doses are given as three separate boluses with a minute in between doses with continuous ECG monitoring to see the effects.
What should you warn the patient about regarding the side effects of adenosine? (tick all that apply)
After three doses of IV adenosine, Sally’s cardiac monitor shows that she is in sinus rhythm at a rate of 110bpm.
You request an ECG to confirm this:
Image: MIAMI group. Courtesy of ivimeds.org
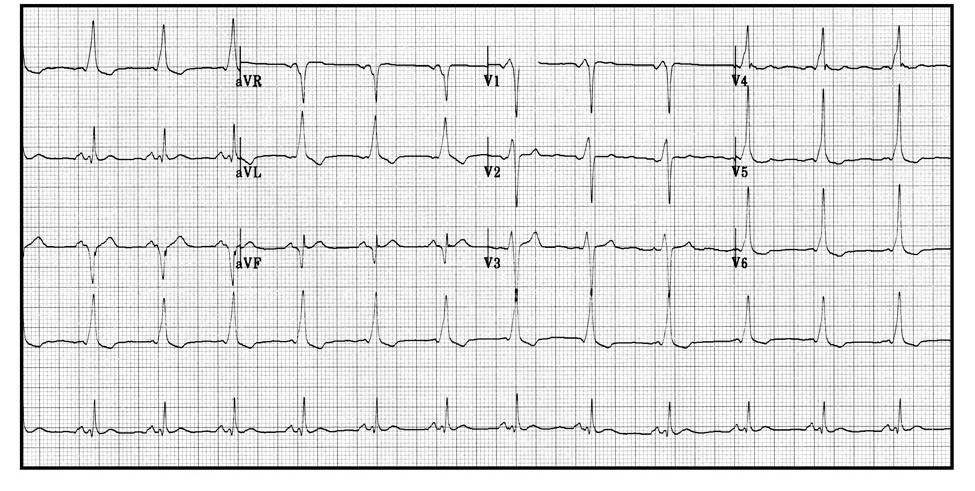
Look at the shape of the QRS complex. What does the ECG show?
The ECG shows sinus rhythm with DELTA waves present. i.e. the first part of the QRS complex has the same slopey shape as Concord's wing.
Here is a difficult question: What is the most likely diagnosis from reviewing Sally’s ECG?
Why would a history of asthma be relevant when thinking about possible drug treatment for this scenario?
There are some cardiac drugs that are contraindicated in asthma because they can cause broncho constriction e.g. beta-blockers, adenosine. It is worth asking now rather than dealing with an additional asthma attack later!
In the interview you hear how Dr Ann Chu managed a patient in this situation:
(Broadband required, click the buttons to play and pause the audio)
1 - Adenosine Pharmacology
Adenosine
Is this the same adenosine that is part of the Krebs cycle that feature in school biology lessons?
Yes, adenosine is a naturally occurring substance inside the cells of the body. It has an important action on the AV node when given intravenously.
Listen to the audio on the pharmacodynamics of adenosine.
There are questions and hesitations in the recording: If you want to you can stop the recording and "fill" them in.
Standard dose:
Drug interactions with adenosine:
Contra-indications:
Answer the questions during or after listening to the audio clip.
The half life of adenosine in the blood is ...?
What factors can increase the risk of an adverse reaction such as heart block or an other arrhythmia occuring when giving adenosine?
Interactions with other drugs, such as Diltiazem and Verapamil (Some types of calcium channel blockers), amiodarone and others.
Electrolyte imbalances such as low potassium and magnesium.
Select the most accurate description of the mechanism of action of adenosine...
Adenosine is antagonized by xanthines, a drug group which includes theophylline and caffeine.
What might happen to the dose requirement if the patient has just drunk a can of red bull prior to presenting the Emergency department with a feeling of their heart racing?
The drug Dipyridamole is given to people who have had Transient Ischaemic Attacks (TIA) or a stroke in order to cause vasodilatation of small blood vessels in the brain to increase collateral perfusion.
It delays the uptake of adenosine into the cells of the vascular endothelium.
How will you have to change the dose if your patient is on dypyridamole and has developed a supra-ventricular tachycardia?
1 - Observation
The medical registrar advises that she be kept on a cardiac monitor overnight and to refer to the cardiology team in the morning.
You check the results of the blood tests:
Hb 12.7
WCC 7.8
Plt 225
Na 141
K 3.2
Urea 4.2
Cr 89
Clotting: normal
Other biochemistry: normal
What is abnormal? and what would you do about it?
A level of 3.2 is not very low and oral supplementation is appropriate if the patient can take, retain and absorb oral nutrients.
You need to ask yourself if there is a reason for the low potassium level. This could increase the risk of prescribing certain cardiac medications, such as fleicanide, but also others such as digoxin. (see the learning exercise on this drug).
2 - Debrief Information
What is Wolff-Parkinson-White syndrome?
It is caused by a congenital accessory conduction pathway between the atria and ventricles.
You could explain it like this: "Sally was born with an extra connection between the chambers of her heart. Usually there is only one connection between the top chambers and the bottom chambers, which acts as a safety mechanism and stops the heart from beating too fast. In her case, the extra connection bypasses the safety mechanism”
The cardiology registrar has told Sally that Wolff-Parkinson-White can lead to sudden death.
How can sudden death occur in Wolf Parkinson White patients if the enter atrial fibrillation?
In atrial fibrillation, the AV node plays a large role in controlling the ventricular rate. If a patient with an accessory pathway (as in WPW) develops AF, the ventricles are not protected by the AV node. This leads to ventricular fibrillation and sudden death.
ECG showing atrial fibrillation in Wolff-Parkinson-White syndrome

Follow-up - Follow-up
Sally is discharged with flecainide (“pill in the pocket”) whilst awaiting her ablation surgery.
The flecainide is only for use if she enters a tachycardia again whilst at home/work in the meantime.
What do I need to know about Flecainide?
Not much, you would not prescribe it by yourself. You need to be aware that it is an anti arrhythmic medication that can prevent and treat supra ventricular tachycardia. It is generally used only in fitter patients without other heart diseases.
Adverse reactions include effects on the central nervous system (Drowsiness, etc) and pro-longation of the cardiac Q T interval especially in cases of hypokalaemia and poor left ventricular function.
Extreme caution should be used when medication(s) affecting cardiac conduction is already used by the patient.
Which medication would you LEAST want to risk an interaction with by giving flecainide?
Follow-up - Bibliography
Latest Edit: Febuary 2011
Bibliography
Hampton JR. (2000) The ECG Made Easy. 5th edition. Churchill Livingstone.
Longmore et al. (2007) Oxford Handbook of Clinical Medicine 7th edition. OUP.
UK Resuscitation Council Guidelines (2010) Adult Life Support, Adult Tachycardia and Adult Bradycardia algorithms
Grahame-Smith & Aronson, J. Oxford Textbook of Clinical pharmacology and drug therapy. 3rd edition. OUP.